Improving Transparency and Accountability in Funding Decisions
Improving Transparency in Funding Allocation
Transparency in funding allocation is crucial for maintaining public trust and ensuring the responsible use of resources in medical research. A transparent process allows stakeholders to understand the criteria used to select research projects, the rationale behind funding decisions, and the potential impact of those decisions on the overall advancement of medical knowledge. This includes detailed explanations of the evaluation process, clear guidelines for the submission of proposals, and readily accessible information on the awarded projects, including summaries of their aims, methodologies, and anticipated outcomes. This transparency fosters accountability and allows for meaningful scrutiny of the funding process, thereby minimizing potential bias and maximizing the likelihood of impactful research.
Implementing robust data management systems and utilizing readily available, standardized reporting protocols are key components of achieving this transparency. Such systems should allow for easy access to historical funding data, enabling researchers and the public to identify trends and patterns in the allocation of resources. Moreover, fostering open communication channels between funding agencies, researchers, and the public will contribute significantly to a more transparent and accountable system. This includes providing opportunities for feedback on the funding process and ensuring that all stakeholders have the means to understand the rationale behind the decisions made.
Ensuring Accountability in Grant Management
Accountability in grant management is essential for upholding the integrity of medical research funding. This necessitates rigorous oversight mechanisms that track the use of funds, monitor the progress of research projects, and ensure compliance with established ethical guidelines and regulations. Clear reporting requirements for researchers regarding the expenditure of funds and the achievement of project milestones are vital components of this accountability framework. This necessitates a culture of responsibility within both the research institutions and the funding agencies, which fosters a commitment to ethical conduct and prevents potential misuse of resources.
Furthermore, independent audits and reviews of the grant management process can provide valuable insights into the effectiveness of current procedures and identify areas for improvement. Regular evaluation of the impact of funded research on patient care and public health is crucial for ensuring that resources are allocated efficiently and effectively. This includes establishing metrics for measuring the impact of research projects and making this data publicly available. This approach allows for a comprehensive assessment of the return on investment for funding decisions and promotes accountability for the outcomes of the research.
Establishing clear procedures for addressing potential conflicts of interest, ensuring compliance with data privacy regulations, and implementing robust mechanisms for handling complaints and grievances are also critical aspects of ensuring accountability. These mechanisms must be transparent, accessible, and impartial to allow for the efficient resolution of any issues that may arise, maintaining the integrity of the entire process. Implementing such measures fosters trust and confidence in the medical research community and the funding agencies.
The Future of AI in Medical Research Funding: Challenges and Opportunities
Funding Models for AI in Medical Research
Securing adequate funding is crucial for advancing AI in medical research. Current funding models, often focused on traditional research methodologies, may not fully capture the unique needs and complexities of AI projects. This necessitates a shift towards more flexible and adaptable models. For example, grants specifically designed for AI-driven medical research could encourage multidisciplinary collaborations and provide seed funding for innovative projects. This could involve partnerships between research institutions, pharmaceutical companies, and technology startups, fostering a dynamic ecosystem for AI development in healthcare.
Furthermore, exploring alternative funding mechanisms, such as venture capital investments tailored to medical AI, could help bridge the gap between research and commercialization. Such investments would target projects with clear commercial potential, accelerating the translation of research findings into practical applications for patient care. This approach could attract private sector participation and provide the long-term financial support necessary for sustained progress in the field.
Addressing Ethical and Regulatory Concerns
The rapid advancement of AI in medical research raises significant ethical considerations that must be addressed proactively. These include issues of data privacy, algorithmic bias, and transparency in AI systems. Robust ethical guidelines and regulations are essential to ensure responsible development and deployment of AI tools in healthcare. This includes establishing clear protocols for data collection, storage, and usage, and implementing mechanisms to mitigate bias in algorithms. Furthermore, ongoing dialogue among researchers, ethicists, policymakers, and the public is crucial for shaping ethical frameworks that balance innovation with societal values.
Regulatory hurdles also pose challenges for AI-based medical research. Navigating existing regulations governing medical devices and clinical trials can be complex and time-consuming for AI-focused projects. Streamlining regulatory processes and developing specific guidelines for AI medical devices could accelerate the development and adoption of these technologies. This could involve collaboration between regulatory bodies and technology developers to ensure that AI tools are safe, effective, and compliant with established standards.
Data Access and Infrastructure
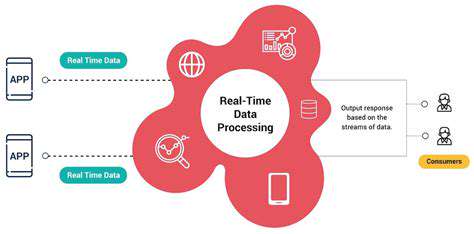
Access to high-quality, diverse, and reliable data is critical for training and validating AI models in medical research. However, data silos and limitations in data sharing can hinder progress. Establishing robust data infrastructure and promoting data sharing initiatives are essential for fostering collaboration and accelerating research. This could involve creating national or international data repositories specifically designed for AI in medicine, ensuring data security and privacy while maximizing accessibility for researchers.
Investment in advanced computing infrastructure is also crucial. AI models often require significant computational resources. Researchers need access to powerful computing clusters and cloud-based platforms to handle the complex data analysis and model training required for cutting-edge AI research. Funding initiatives that support the development and maintenance of these essential resources will be vital for the future of AI in medical research.
Collaboration and Knowledge Transfer
Successful implementation of AI in medical research requires strong collaborations between researchers, clinicians, and industry partners. Cross-disciplinary teams combining expertise in medicine, computer science, and engineering are crucial for developing effective and impactful AI solutions. Facilitating these collaborations through funding opportunities and dedicated research programs can foster innovation and knowledge transfer. This includes establishing platforms that connect researchers with clinicians and industry stakeholders, enabling them to work together on shared challenges and opportunities.
Furthermore, promoting knowledge transfer from research to practice is essential. Effective communication channels and training programs for clinicians on the use of AI tools are crucial for ensuring that these innovations are integrated into routine patient care. This can involve developing educational materials, workshops, and mentorship programs to support the adoption of AI-driven tools and techniques across healthcare settings.