Personalized Treatment Recommendations and Risk Stratification

Personalized Treatment Recommendations: A New Era in Healthcare
Personalized treatment recommendations are revolutionizing the healthcare landscape, moving away from a one-size-fits-all approach to a more tailored and effective method of patient care. This shift is driven by advancements in medical technology, genomic research, and data analysis, allowing healthcare providers to consider individual patient factors when developing treatment plans. This personalized approach promises improved outcomes and reduced side effects by targeting therapies specifically to the needs of each patient.
By analyzing a patient's unique genetic makeup, medical history, lifestyle, and environmental factors, clinicians can identify specific vulnerabilities and strengths that influence their response to various treatments. This allows for the selection of therapies most likely to be effective and well-tolerated, ultimately improving patient quality of life and reducing the burden of disease.
Tailoring Treatment for Optimal Results
The cornerstone of personalized treatment recommendations lies in the ability to tailor interventions to the individual. This approach considers not only the disease itself but also the patient's specific characteristics. These characteristics include age, pre-existing conditions, lifestyle choices, and even environmental factors. Understanding these nuances enables healthcare professionals to predict treatment responses and potential side effects with greater accuracy. This targeted approach offers a more precise and effective strategy for managing and potentially curing various health conditions.
Furthermore, personalized medicine empowers patients to actively participate in their healthcare decisions. By understanding the rationale behind their treatment plan, patients can make more informed choices and collaborate more effectively with their healthcare team. This collaborative approach fosters a more proactive and empowering relationship between patients and their providers.
The Future of Healthcare: Precision Medicine
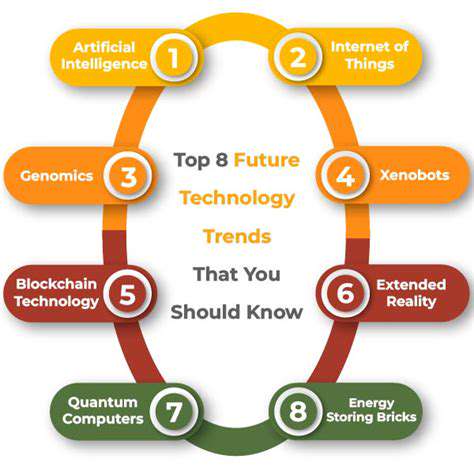
The future of healthcare is deeply intertwined with the concept of precision medicine. This emerging field focuses on using genomic and other data to predict individual responses to treatments, ultimately leading to more effective and personalized therapies. By harnessing the power of advanced technologies and data analysis, precision medicine aims to develop treatments tailored to each patient's unique genetic profile and clinical presentation. This approach is expected to significantly improve health outcomes, reduce healthcare costs, and empower patients to take a more active role in their own care.
The application of precision medicine extends beyond individual diagnoses and treatment plans to encompass public health initiatives. By identifying genetic predispositions to certain diseases within populations, public health professionals can implement targeted preventive strategies to minimize the risk of these conditions.
The Future of AI in CDSS: Challenges and Opportunities

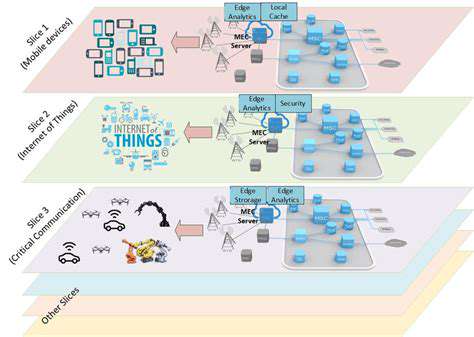
The Growing Need for AI Integration
The increasing complexity of clinical data and the ever-expanding volume of patient information are pushing the boundaries of traditional clinical decision support systems (CDSS). Traditional CDSS often struggle to sift through this mountain of data effectively and provide timely, accurate insights. This necessitates the integration of AI to automate tasks, analyze data patterns, and ultimately, enhance the quality and efficiency of medical care.
AI's ability to process and interpret vast datasets far surpasses human capabilities, leading to more comprehensive and accurate diagnoses. Integrating AI into CDSS can unlock the potential for earlier detection of diseases and improve patient outcomes by generating more personalized treatment plans.
Addressing Data Quality and Bias
One of the primary challenges in implementing AI-powered CDSS is ensuring the quality and reliability of the data used for training and operation. Inaccurate or incomplete data can lead to biased algorithms and inaccurate predictions, potentially harming patient care. It is crucial to establish robust data governance and quality control measures to mitigate these risks.
Addressing potential biases in the data is paramount to ensuring fairness and equity in AI-powered CDSS. Careful consideration must be given to the representation of diverse patient populations to avoid perpetuating existing health disparities. This requires ongoing monitoring and evaluation of the system's performance across various demographics.
Developing Ethical Frameworks for AI in Healthcare
The integration of AI into CDSS raises significant ethical considerations regarding patient privacy, data security, and accountability. Robust data security protocols must be implemented to protect sensitive patient information from unauthorized access or breaches. Maintaining transparency in AI algorithms is vital to building trust and ensuring that clinicians understand how the system arrives at its recommendations.
Clear ethical guidelines and regulations are essential to govern the development and deployment of AI in healthcare. This includes establishing mechanisms for accountability in cases where AI-driven recommendations lead to adverse outcomes. Ongoing dialogue between healthcare professionals, ethicists, and policymakers is critical to navigate these complex ethical considerations.
Ensuring Seamless Integration and User Adoption
A successful implementation of AI-powered CDSS hinges on a smooth integration process that seamlessly incorporates the new technology into existing workflows. This requires careful planning, training, and support for clinicians to effectively utilize the system's features and interpret its outputs. Clinicians need to be empowered with the knowledge and tools to understand and critically evaluate AI-generated recommendations.
User adoption and acceptance are crucial for the long-term success of AI-powered CDSS. User-friendly interfaces, clear documentation, and ongoing support are essential to ensure that clinicians feel comfortable and confident using the system. This will ultimately improve the quality of care and efficiency of clinical workflows.