Personalized Medication Management: Optimizing Outcomes for Children

Understanding Your Medication Needs
Personalized medication management goes beyond simply taking your prescribed pills. It's a proactive approach to understanding your individual health needs and how different medications interact with your body and lifestyle. This involves careful consideration of your medical history, current health conditions, and any potential allergies or sensitivities. By understanding these factors, you can work with your healthcare provider to develop a medication plan that's tailored to your specific requirements and promotes optimal health outcomes.
A thorough understanding of your medications is crucial. This includes knowing the purpose of each medication, the recommended dosage, and the potential side effects. It also involves understanding how different medications might interact with each other or with other supplements or foods you might consume. This proactive knowledge empowers you to communicate effectively with your healthcare team and make informed decisions about your health.
Creating a Structured Medication Routine
Developing a structured medication routine is essential for effective management. This means establishing a consistent schedule for taking your medications, ideally at the same time each day. This helps to ensure that your body receives the necessary medication doses at the appropriate intervals. This consistent approach also reduces the risk of forgetting doses, a common issue that can negatively impact your health.
Using medication organizers, pill boxes, or mobile apps can be incredibly helpful. These tools provide a visual reminder of when to take each medication, preventing missed doses and promoting adherence to your prescribed regimen. They also help to keep track of your medication history, providing valuable information for your healthcare providers.
Monitoring Your Medication's Impact
Monitoring the impact of your medications is critical for ensuring their effectiveness and safety. This includes noting any potential side effects, such as nausea, headaches, or skin rashes. Regular communication with your healthcare team about any observed changes in your health is vital for adapting your medication plan as needed. This ensures that your medication regimen remains optimal and addresses any emerging health concerns promptly and effectively.
Tracking your symptoms and how your body responds to the medications is important. This allows you to identify potential issues early on and enables you to modify your treatment plan with the guidance of your healthcare provider if necessary. This active involvement in your health management is key to achieving positive outcomes.
Seeking Professional Guidance
Ultimately, personalized medication management requires ongoing collaboration with your healthcare providers. Regular check-ups and consultations are crucial to assess the effectiveness of your current medication regimen and to make any necessary adjustments. Maintaining open communication with your doctor ensures that your medication plan remains tailored to your evolving health needs and addresses any emerging health concerns.
Don't hesitate to ask questions about your medications. Understanding the reasoning behind each medication, its potential side effects, and how it interacts with other treatments is essential for informed decision-making. This proactive approach to your health empowers you to take an active role in managing your health and well-being.
Ethical Considerations and Future Directions: Navigating the Landscape of AI in Pediatrics
Data Privacy and Security
Protecting the sensitive health information of children is paramount. AI systems used in pediatric care must adhere to the strictest data privacy regulations, such as HIPAA and GDPR, ensuring anonymization, secure storage, and access controls. Robust mechanisms for data encryption and secure transmission protocols are crucial to prevent unauthorized access and breaches. Furthermore, transparent data usage policies should be established and communicated clearly to parents and patients, outlining how their information will be collected, used, and protected.
Bias Mitigation and Fairness
AI algorithms trained on historical data can inadvertently perpetuate existing biases, potentially leading to disparities in diagnosis and treatment recommendations for children from different backgrounds. Careful consideration must be given to the data sources used for training, and ongoing monitoring and evaluation are essential to identify and rectify biases. This involves diverse data sets, rigorous testing protocols, and the development of methods to assess and mitigate potential biases in AI algorithms.
It's critical to ensure that AI systems are fair and equitable in their application, avoiding discriminatory outcomes based on factors like race, socioeconomic status, or geographic location.
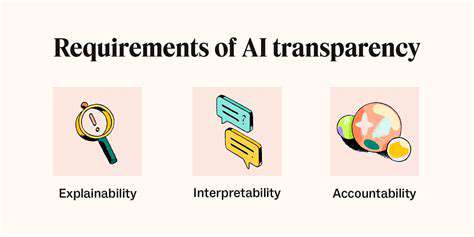
Clinical Validation and Transparency
AI systems employed in pediatric care must undergo rigorous clinical validation to demonstrate their efficacy and safety. This involves rigorous testing in controlled settings, comparison with established clinical practices, and the demonstration of clinical utility. Transparency in the decision-making processes of AI systems is equally important. Explanations of how AI systems arrive at their conclusions should be readily available, enabling clinicians to understand and interpret the rationale behind recommendations.
Patient Autonomy and Informed Consent
Children's rights to autonomy and participation in decision-making must be respected. As AI plays a growing role in their healthcare, methods for engaging children and adolescents in discussions about AI-driven interventions must be developed. This includes educating them about the technology and its potential benefits and risks. Obtaining informed consent from parents and, where appropriate, involving the child in the process is essential. This process should respect the developmental stage and capacity of the child.
Healthcare Professional Training and Education
Clinicians need adequate training and education to effectively utilize AI tools in pediatric care. This includes understanding the strengths and limitations of AI systems, how to integrate them into existing workflows, and how to critically evaluate the output of AI algorithms. Continued professional development opportunities should be available to keep healthcare professionals up-to-date on advancements in AI and its applications in pediatrics.
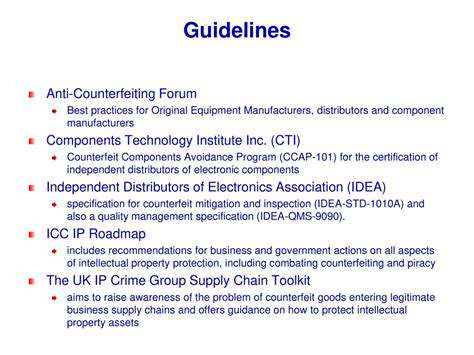
Ethical Oversight and Regulation
Robust ethical oversight mechanisms are needed to guide the development and implementation of AI in pediatric healthcare. Independent review boards and ethical committees should play a crucial role in evaluating the ethical implications of AI applications and ensuring compliance with relevant regulations. This includes establishing clear guidelines and best practices for the design, development, and deployment of AI systems in pediatric care. Ongoing dialogue and collaboration among stakeholders, including clinicians, researchers, ethicists, policymakers, and patients, is vital.
Long-Term Impact and Societal Considerations
The long-term societal impact of AI in pediatric care needs careful consideration. Potential impacts on healthcare access, equity, and the future of pediatric practice must be evaluated. Ongoing research and evaluation are crucial to understanding the evolving role of AI in shaping the future of pediatric healthcare. A holistic approach, considering the impact on families, communities, and society as a whole, is essential in navigating the future of AI in this field.