Improving Patient Outcomes and Reducing Recovery Time
Improving Patient Outcomes Through Enhanced Communication
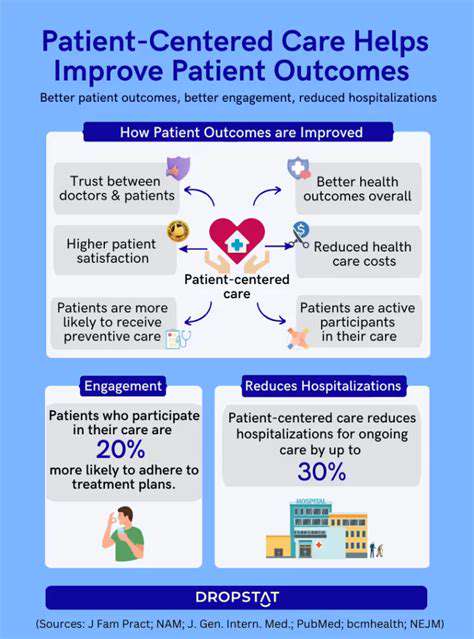
Effective communication between healthcare professionals and patients is paramount to improving patient outcomes. Clear, concise, and empathetic communication fosters trust and understanding, enabling patients to actively participate in their care. This collaborative approach allows for a more comprehensive understanding of individual needs and preferences, ultimately leading to better adherence to treatment plans and improved health outcomes.
Open dialogue and active listening are crucial components of this process. Healthcare providers should actively seek to understand the patient's perspective, concerns, and expectations. This involves not only asking questions but also actively listening to the responses, acknowledging their emotions, and ensuring that patients feel heard and respected.
Addressing Systemic Barriers to Patient Care
Beyond individual interactions, systemic barriers within the healthcare system can significantly impact patient outcomes. These barriers can include inadequate access to resources, logistical challenges in scheduling appointments, and inconsistencies in the quality of care provided across different facilities. Addressing these issues requires a multifaceted approach involving policy changes, improved infrastructure, and enhanced coordination between healthcare providers.
Streamlining processes and improving efficiency can significantly reduce wait times and increase patient satisfaction. This, in turn, can lead to a more positive patient experience and potentially better adherence to treatment plans.
Furthermore, fostering a culture of continuous quality improvement within healthcare settings is essential. Regular evaluations, feedback mechanisms, and a commitment to learning from both successes and failures are crucial for identifying and rectifying systemic issues that may hinder patient progress.
Tailoring Treatment Plans to Individual Needs
Effective treatment plans must be tailored to the unique needs and circumstances of each individual patient. This involves considering various factors, including their medical history, lifestyle choices, socioeconomic status, and personal preferences. A personalized approach recognizes that patients are not merely diagnoses but complex individuals with diverse needs and requirements.
By understanding the patient's specific context, healthcare providers can develop interventions that are more likely to be successful. This personalized approach can enhance patient engagement and motivation, leading to better adherence to prescribed therapies and improved overall health outcomes.
Enhancing Patient Education and Empowerment
Empowering patients with knowledge and resources is critical to fostering their active participation in their own care. Comprehensive patient education programs can provide valuable information about their conditions, treatment options, and potential side effects. Clear and accessible information empowers patients to make informed decisions and actively participate in their care.
Providing patients with the tools and resources to manage their health effectively can greatly improve their outcomes. This includes access to reliable information, educational materials, and support systems. Ultimately, empowering patients fosters a sense of ownership and control over their health journey, leading to improved adherence and better overall well-being.
By encouraging patients to ask questions, actively participate in decision-making, and understand their treatment plan, healthcare providers can create a supportive environment that promotes positive health outcomes.
The Future of AI in Robotic-Assisted Physical Therapy
Personalized Rehabilitation Plans
AI-powered systems can analyze patient data, including medical history, physical assessments, and treatment responses, to generate personalized rehabilitation plans. This tailored approach ensures that each patient receives the most effective and efficient treatment, maximizing their recovery potential. By considering individual factors like muscle strength, range of motion, and pain tolerance, AI algorithms can dynamically adjust exercise routines and treatment protocols, leading to more effective and personalized outcomes.
These personalized plans will go beyond pre-set routines. AI will be able to adapt to real-time feedback from the patient and the robotic system, adjusting exercises and intensity to maintain optimal progress. This dynamic approach will significantly improve the effectiveness of physical therapy, as it's tailored to the specifics of each patient's recovery journey.
Enhanced Safety and Efficiency
Robotic systems guided by AI algorithms can precisely monitor patient movements and provide real-time feedback to therapists. This real-time assessment significantly enhances the safety of the therapy process, preventing overexertion or improper form that could hinder recovery or cause injury. The data collected by the AI can also assist therapists in identifying potential risks or complications early on, allowing for immediate intervention and preventing further issues.
Moreover, AI can optimize the efficiency of robotic-assisted physical therapy. By automating routine tasks and providing real-time data analysis, AI can reduce the time therapists spend on manual tasks. This allows therapists to focus more on patient interaction and provide more personalized attention to their needs, ultimately accelerating the healing process.
Improved Accessibility and Affordability
AI-driven robotic systems could potentially make physical therapy more accessible to a wider range of individuals, particularly those in remote areas or with limited access to qualified therapists. Remote monitoring and virtual consultations enabled by AI could significantly improve access to care, allowing patients to receive guidance and support even when traditional therapy sessions are not feasible. This broader accessibility will be a key factor in improving public health outcomes.
Advanced Diagnostics and Prognosis
AI can analyze the data collected during robotic therapy sessions to identify subtle patterns and trends that might indicate the presence of underlying issues or predict potential complications. This proactive approach to diagnosis could lead to earlier intervention and more effective treatment strategies. AI algorithms can also analyze patient data to develop more accurate prognoses, allowing therapists and patients to better plan for the recovery journey and set achievable goals.
By predicting possible future challenges, AI can help therapists and patients adjust their approach proactively. This anticipatory ability to identify potential problems and adjust treatment strategies will contribute significantly to the overall success and safety of the robotic-assisted therapy process.
Integration with Wearable Technologies
Integrating AI with wearable sensors and other patient-monitoring devices creates a comprehensive data collection system. This combined data stream allows for a more holistic view of the patient's progress, providing insights into their overall physical condition and treatment response. Real-time monitoring of vital signs and activity levels, combined with the data from robotic therapy, will provide a more complete picture of the patient's condition.
This integration will allow for a more proactive and personalized approach to care, enabling therapists to adjust treatment plans based on real-time data and individual patient needs, thereby improving the effectiveness of rehabilitation.