Introduction to AI in Kidney Disease Diagnosis
Early Detection and Prevention
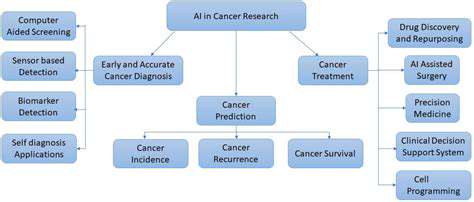
Modern advancements in artificial intelligence are transforming how we approach kidney disease diagnosis, providing opportunities for earlier identification and more effective preventative strategies. By examining extensive datasets that include patient medical histories, laboratory findings, and imaging results, AI-driven systems can detect nuanced patterns and risk indicators that clinicians might overlook. This capability enables timely medical interventions that can slow or even prevent the progression of kidney disease, leading to significantly better health outcomes for patients.
One of the most valuable applications is predicting an individual's likelihood of developing kidney disease. Through sophisticated modeling, AI can highlight high-risk patients based on their unique profiles, allowing for preemptive measures such as lifestyle adjustments and early medical care. These steps can be pivotal in reducing the chances of the disease taking hold.
Improved Diagnostic Accuracy
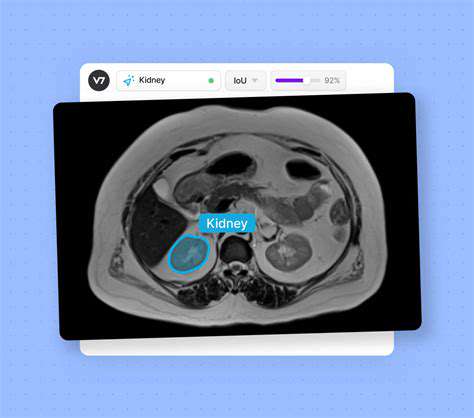
AI systems are particularly adept at spotting subtle irregularities in medical imagery, such as X-rays and ultrasound scans, which may elude even trained eyes. This heightened precision is especially important in kidney disease diagnosis, where early stages often present with minimal or no symptoms. By scrutinizing kidney structures in detail, AI can identify potential issues like cysts, tissue damage, or impaired blood circulation, paving the way for earlier treatment and better management of the condition.
Personalized Treatment Strategies
Another groundbreaking application of AI lies in crafting tailored treatment plans for kidney disease patients. By leveraging individual health data, AI can design therapies that maximize effectiveness while minimizing adverse effects. This bespoke approach takes into account the specific type of kidney disease, the patient's overall health status, and their previous responses to treatments. Such customization is vital for optimizing therapeutic outcomes and reducing complications.
Automated Data Analysis and Reporting
AI also excels in processing large datasets swiftly and accurately, drastically cutting down the time needed for diagnosis. This automation allows healthcare providers to dedicate more time to direct patient care, facilitating deeper consultations and more personalized treatment strategies. Additionally, AI's ability to generate automated reports ensures that critical diagnostic information is relayed efficiently to the relevant medical professionals.
Enhanced Efficiency in Clinical Trials
The integration of AI into kidney disease research can significantly boost the efficiency of clinical trials. By automating data collection and analysis, AI accelerates the identification of promising treatments and the monitoring of patient responses. This efficiency enables researchers to explore a broader range of therapeutic options, ultimately speeding up medical advancements and improving patient care.
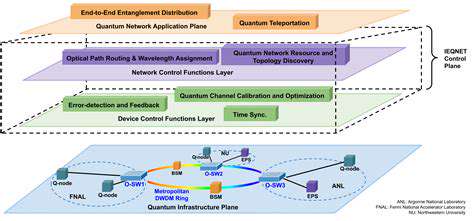
Integration with Existing Healthcare Systems
For AI to be truly effective in kidney disease diagnosis, it must integrate seamlessly with current healthcare infrastructures. This requires robust interfaces and stringent data security measures to ensure the safe handling of patient information. The incorporation of AI tools into clinical workflows must be thoughtfully executed to enhance, rather than disrupt, existing practices. A smooth transition is essential to maintain the integrity and efficiency of healthcare delivery.
Ethical Considerations and Future Directions
The deployment of AI in diagnosing kidney disease brings to light important ethical issues, particularly concerning data privacy and the potential for algorithmic bias. It is imperative that AI systems are trained on diverse datasets to prevent the reinforcement of existing health inequalities. Future research should prioritize addressing these challenges while refining AI technologies to ensure they are both precise and fair. Continued innovation in this field is crucial for improving diagnostic accuracy, streamlining processes, and enhancing patient care, all while upholding ethical standards.
Predictive Modeling for Early CKD Detection
Understanding the Importance of Early Detection in CKD
Chronic Kidney Disease (CKD) often progresses silently, making early detection a critical factor in effective management. Predictive modeling has emerged as a powerful tool for identifying individuals at high risk before irreversible kidney damage occurs. By evaluating a combination of clinical, demographic, and laboratory data, healthcare providers can implement targeted interventions to slow disease progression. Early identification enables lifestyle changes, medication adjustments, and close monitoring—key strategies in managing chronic conditions.
Advances in predictive analytics have led to the creation of sophisticated algorithms capable of assessing multiple risk factors at once. These models consider variables such as blood pressure, glucose levels, age, and genetic predispositions to generate comprehensive risk assessments. Intervening early based on these insights can dramatically improve patient outcomes and alleviate the strain on healthcare resources. Integrating predictive models into standard clinical practices helps medical professionals make data-driven decisions, leading to more personalized care and efficient resource use.
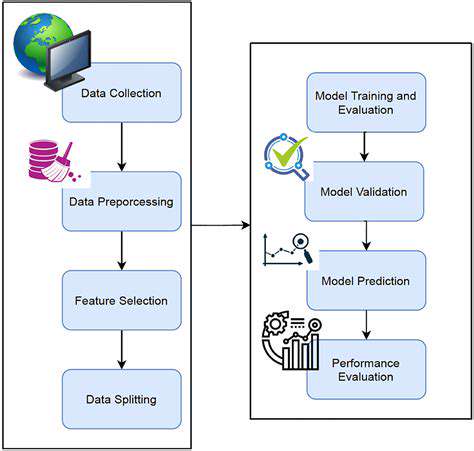
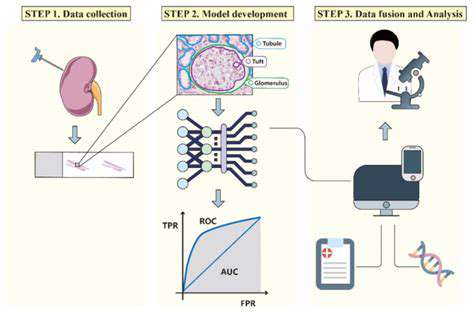
Techniques and Data Sources in Predictive Modeling for CKD
Predictive modeling for CKD employs a range of statistical and machine learning methods, including logistic regression, decision trees, random forests, and neural networks. Each technique offers distinct advantages in analyzing complex datasets and uncovering hidden patterns. Selecting the right approach depends on the data's nature, the clinical questions at hand, and the desired level of predictive accuracy. The effectiveness of these models is heavily influenced by the quality and breadth of the data sources used. Common data inputs include electronic health records (EHR), lab results, imaging data, and patient-reported information.
Data preprocessing—cleaning, normalizing, and selecting relevant features—is essential for optimizing model performance. Advanced models also utilize longitudinal data to track trends over time, enhancing their predictive power. Collaboration among data scientists, clinicians, and researchers is key to developing models that are both accurate and clinically relevant. With technological advancements, integrating real-time data from wearable devices presents exciting opportunities for continuous risk monitoring and proactive CKD management.
AI-Assisted Differential Diagnosis of Kidney Disorders
Leveraging AI for Enhanced Diagnostic Accuracy
Artificial intelligence is making significant strides in healthcare, particularly in improving diagnostic processes. AI-powered tools can sift through vast amounts of medical images, patient records, and other pertinent data to uncover subtle patterns that might escape human detection. This enhanced analytical capability leads to more accurate and often quicker diagnoses, which can be lifesaving in critical situations.
Automating the analysis of complex data with AI can drastically reduce the time needed to reach a diagnosis. This is especially valuable in emergencies where swift action is required. When integrated effectively into clinical workflows, AI-driven diagnostics have the potential to revolutionize patient care by combining speed with precision.
Improving Efficiency and Reducing Bias
AI can streamline diagnostic workflows by automating tasks like image analysis and data interpretation. This allows clinicians to focus on more nuanced aspects of patient care, such as building relationships and providing comprehensive support. Such efficiency gains are particularly beneficial in settings with limited resources.
AI also has the potential to reduce human bias in diagnosis. By relying on objective data analysis, AI systems can minimize the impact of subjective judgments, leading to more consistent and fair diagnostic outcomes. This is especially important in diverse populations where unconscious biases may influence clinical decisions.
Addressing Limitations and Ensuring Ethical Considerations
While AI-assisted differential diagnosis holds great promise, it is important to recognize its limitations and address ethical concerns. AI models are only as good as the data they are trained on, and biased data can lead to biased outcomes. Rigorous validation and continuous monitoring are essential to ensure the fairness and accuracy of AI tools.
Transparency in how AI algorithms make decisions is crucial for building trust and ensuring accountability. Additionally, robust measures must be in place to protect patient privacy and data security, maintaining confidentiality and integrity throughout the diagnostic process.
Personalized Medicine and Tailored Treatment Plans
AI-assisted diagnosis can pave the way for more personalized healthcare. By analyzing individual patient data, AI can identify specific risk factors and recommend treatments tailored to each person's unique needs. This approach not only improves treatment efficacy but also reduces the likelihood of adverse effects.
The ability to create customized treatment plans based on detailed patient data is one of the most significant benefits of AI in healthcare. This shift toward personalized medicine has the potential to improve outcomes and foster a more proactive approach to health management.
Future Directions and Research
The field of AI-assisted differential diagnosis is rapidly evolving, with ongoing research aimed at improving accuracy, efficiency, and ethical safeguards. Future developments may include more advanced algorithms and the integration of diverse data sources, such as genomic data and real-time information from wearable devices.
Incorporating a wider range of data sources, including genomics and wearable technology, could provide a more holistic view of patient health. Continued research, coupled with careful attention to ethical concerns, will ensure that AI remains a valuable tool in enhancing diagnostic precision and patient care.