Harnessing Big Data for Disease Prediction
Improving Diagnostic Accuracy
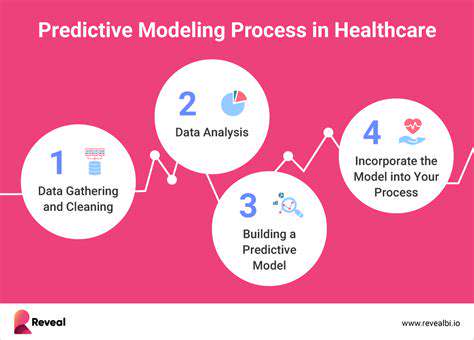
The utilization of extensive datasets enables the creation of advanced computational models capable of processing enormous volumes of patient information. This encompasses medical records, lifestyle choices, genetic markers, and environmental factors. Such thorough examination can reveal subtle connections that conventional diagnostic approaches might overlook, thereby enhancing both the precision and speed of medical assessments. Through these complex data analyses, healthcare providers gain deeper insights into disease development, allowing for more customized treatment plans and improved patient prognoses.
Examining vast amounts of data facilitates the detection of risk indicators and early symptoms that smaller datasets might miss. This forward-thinking method in disease forecasting enables individuals to adopt preventive actions, potentially postponing or even avoiding chronic illnesses altogether. Timely medical intervention, made possible through comprehensive data analysis, can dramatically influence disease control and decrease the necessity for more aggressive, costly treatments later on.
Personalized Treatment Plans
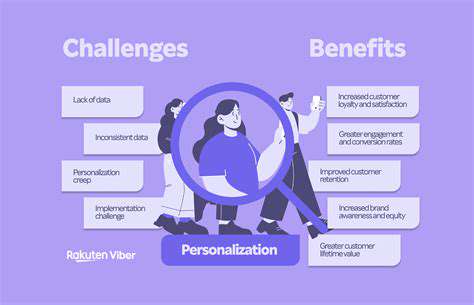
Advanced data analytics permits the customization of medical treatments to suit each patient's specific requirements. By accounting for an individual's genetic profile, daily habits, medical background, and reactions to different therapies, computational models can suggest the most beneficial treatment path. This tailored method not only boosts treatment success rates but also reduces negative side effects, resulting in better health results and enhanced life quality. This patient-specific medical strategy proves particularly vital when addressing complex illnesses demanding multifaceted and flexible approaches.
Additionally, through continuous monitoring of patient data, these systems can evaluate treatment effectiveness and modify approaches as necessary. This adaptable treatment methodology fosters a more responsive healthcare environment, leading to faster recoveries and fewer hospital readmissions. The capacity to observe and fine-tune treatment regimens in real-time offers substantial benefits for both patients and medical professionals, ultimately streamlining the entire treatment process.
The comprehensive nature of data analysis helps identify particular patient traits that might affect their response to specific treatments. This can prevent ineffective therapies and substantially lower healthcare expenses. These analytical tools can also forecast treatment responses and customize medication dosages for optimal effectiveness, reducing trial-and-error approaches and enhancing treatment productivity.
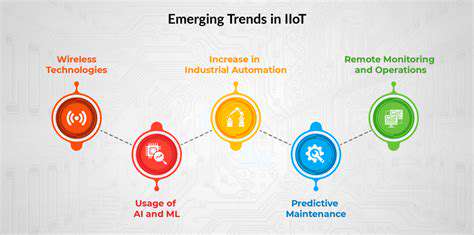
Predictive Modeling for Disease Prevention
By examining historical data regarding disease occurrence, risk elements, and treatment results, computational models can develop forecasting systems that predict an individual's likelihood of contracting specific illnesses. These models can pinpoint high-risk patients and facilitate focused preventive measures that may stop disease onset or progression. This proactive healthcare approach proves essential for lessening the impact of chronic diseases on both individuals and society at large. Early identification and intervention remain crucial for effectively managing long-term health conditions, leading to better overall health and reduced medical expenditures.
Using extensive datasets, researchers can recognize patterns linked to disease outbreaks and anticipate potential future epidemics. This predictive capacity enables health authorities to implement preventive actions and strategies to contain infectious disease spread. The ability to spot emerging disease patterns and execute focused public health initiatives could significantly improve worldwide health outcomes.
Tailoring Preventive Strategies to Individual Needs
Customizing Preventive Approaches for Maximum Effectiveness
Preventive health measures achieve optimal results when specifically designed to meet the distinct requirements and situations of their intended recipients. This individualized strategy considers numerous elements including demographic characteristics, personal habits, environmental factors, and pre-existing medical conditions. Generic, uniform approaches frequently prove inadequate as they may not properly address the particular risks and vulnerabilities of specific groups.
Customized strategies yield superior outcomes by precisely addressing the needs of target populations. This requires thorough comprehension of the unique challenges different communities face and adapting interventions appropriately. Such proactive measures can optimize resource distribution and generate more favorable health results.
Pinpointing Critical Risk Factors for Focused Interventions
Accurate detection of major risk factors remains fundamental for crafting successful preventive measures. These elements span from personal behaviors such as tobacco use and unhealthy eating to broader societal problems including economic hardship and healthcare access limitations. Grasping the complex relationships between these diverse factors proves necessary for developing thorough and impactful solutions.
Meticulous examination of risk factors enables the creation of precisely targeted interventions with higher success probabilities. This procedure involves gathering and analyzing pertinent data to detect patterns and trends associated with particular health concerns.
Creating Research-Backed Preventive Solutions
Preventive approaches must be firmly rooted in scientific evidence to guarantee their efficacy and safety. Comprehensive studies and clinical testing provide the necessary information to justify implementing evidence-based strategies. This ensures efficient resource allocation and increases the likelihood of achieving desired outcomes.
All interventions require comprehensive assessment to determine their effectiveness and possible negative effects. This permits ongoing refinement and adjustment of strategies based on actual implementation results.
Implementing Approaches Across Varied Populations
Successful preventive strategies must demonstrate cultural awareness and accessibility for all intended recipients. This demands understanding and accommodating the special needs and viewpoints of different cultural communities. Considering cultural traditions and beliefs proves essential for ensuring intervention acceptance and compliance.
Cultural sensitivity remains paramount for effective program execution. This involves collaborating with community representatives and stakeholders during both the design and implementation phases of preventive measures.
Tracking and Assessing Program Results
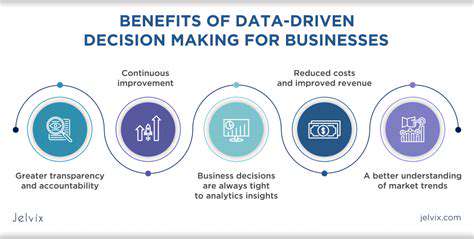
Continuous monitoring and evaluation prove crucial for determining preventive strategy effectiveness. Regular data collection and analysis permit identification of areas requiring enhancement and adjustment of approaches to boost their impact. This cyclical process ensures strategies maintain relevance and effectiveness over extended periods.
Monitoring key performance indicators helps recognize successes and pinpoint areas needing improvement. This evidence-based method allows for constant refinement of interventions, ultimately producing better health outcomes.
Involving Communities in Prevention Efforts
Community participation remains essential for successful implementation and sustainability of preventive strategies. Including community members in program design, execution, and evaluation fosters ownership and responsibility. This cooperative method ensures interventions remain pertinent and valuable to the community.
Enabling communities to actively participate in their health and welfare proves vital for lasting success. This involves providing education opportunities, participation avenues, and decision-making roles within the community framework.
Addressing Economic and Social Inequalities
Preventive approaches must confront socioeconomic factors that frequently contribute to health disparities. These elements include income gaps, educational and resource access limitations, and exposure to environmental dangers. Tackling these inequities proves critical for achieving balanced health results across all demographic groups.
Strategies must account for socioeconomic influences on health and develop specific interventions to counteract these effects. This encompasses policies and programs that enhance economic opportunities and improve access to essential services.
Ethical Considerations and Future Directions
Protecting Patient Information
Safeguarding sensitive health data represents a critical concern in computational disease prediction. Comprehensive protective measures, including data encryption, access restrictions, and anonymization methods, prove essential for preventing unauthorized access and security breaches. Additionally, clear data management policies, specifying how information gets collected, utilized, and stored, remain fundamental for establishing trust and complying with regulations such as HIPAA in the United States and GDPR in Europe. This includes obtaining explicit patient consent regarding data usage for research and predictive modeling purposes.
Addressing Algorithmic Prejudice
Computational models learn from data, and if that data contains societal biases, the resulting predictions may reinforce or even intensify those biases. This could create inequalities in diagnosis and treatment suggestions, potentially harming disadvantaged groups. Consequently, meticulous examination of training data for potential biases becomes imperative. Methods for bias identification and correction should be incorporated throughout development to ensure fairness and equal access to personalized disease prediction.
Regular reviews and testing of models also become necessary to detect and remedy any emerging biases over time. Continuous observation and modifications prove crucial for maintaining impartiality and accuracy as both data and models evolve.
Ensuring Clinical Reliability
The precision and dependability of computational predictions remain vital for medical applications. Extensive validation studies become necessary to demonstrate model reliability across diverse patient groups. This validation should compare computational predictions with established clinical diagnoses and outcomes. Furthermore, models require testing in practical healthcare environments to evaluate performance under various conditions and with different patient demographics.
Promoting Transparency in Decision-Making
Understanding how computational models generate predictions remains essential for clinical acceptance and trust. Opaque algorithms, where the reasoning process remains unclear, prove less acceptable in medical settings. Transparent computational methods should be employed to clarify the factors influencing predictions. This enables medical professionals to better comprehend the basis for predictions and potentially identify areas for model or patient care improvement.
Incorporating Technology into Medical Practice
Successful integration of computational tools into existing medical workflows proves essential for practical implementation. These systems must demonstrate user-friendliness, easy accessibility, and seamless compatibility with electronic health records (EHRs). This reduces strain on medical staff, facilitates efficient data entry, and minimizes potential errors during information input and model application.
Training and education for healthcare providers regarding proper use and interpretation of computational predictions also prove vital for smooth technology integration into clinical settings. Clear protocols and guidelines need establishment for interpreting and applying predictions alongside other diagnostic information.
Safeguarding Vulnerable Groups
Computational prediction models should be developed and implemented with strong emphasis on fairness and accessibility for all population segments. Special consideration must be given to the unique needs and challenges faced by vulnerable groups, including those with limited healthcare access, economic disadvantages, or language barriers. Models require testing and validation across diverse populations to guarantee equitable outcomes.
Establishing Regulatory Guidelines
Creating a definitive regulatory structure proves necessary to oversee the development and implementation of computational disease prediction. This framework should set standards for data protection, security measures, algorithmic fairness, and clinical validity. Cooperation between researchers, medical professionals, policymakers, and regulatory agencies becomes essential to ensure these tools get developed, deployed, and utilized responsibly and ethically.