Introduction to AI in Oncology Treatment Selection
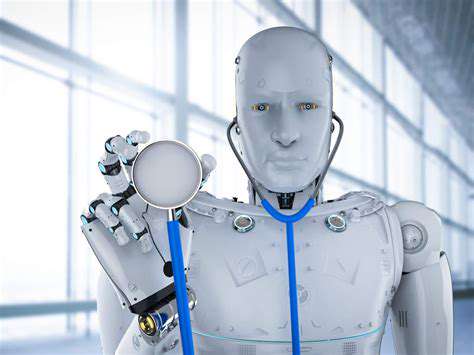
Understanding Artificial Intelligence
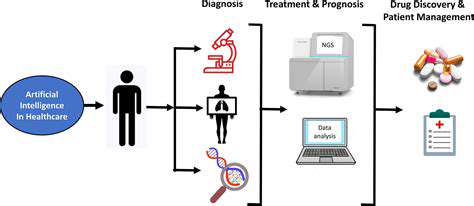
Artificial intelligence (AI) is rapidly transforming various sectors, and oncology is no exception. AI encompasses a broad range of technologies, from machine learning algorithms to deep learning models, capable of analyzing vast amounts of data to identify patterns and make predictions. This allows for more accurate diagnoses, personalized treatment plans, and improved patient outcomes. The potential for AI in oncology is immense and promises to revolutionize the way we approach cancer care.
AI systems are trained on massive datasets of medical images, patient records, and genomic information. Through this training, these systems learn to identify subtle patterns and anomalies that might be missed by human eyes. This capability is particularly valuable in early cancer detection and diagnosis. The ability to analyze massive datasets efficiently is a crucial aspect of AI's promise in healthcare.
AI's Role in Diagnosis and Treatment Planning
AI algorithms can analyze medical images, such as X-rays, CT scans, and MRIs, with remarkable speed and accuracy. They can identify suspicious areas, quantify tumor size, and even predict the likelihood of recurrence. This improved diagnostic accuracy can lead to earlier intervention and more effective treatment strategies. This is especially significant in cases where early detection is crucial for survival.
Beyond diagnosis, AI plays a vital role in tailoring treatment plans. By considering a patient's unique genetic profile, tumor characteristics, and medical history, AI algorithms can suggest optimal treatment options. This personalized approach can lead to more effective therapies and fewer side effects, ultimately improving patient outcomes.
Personalized Medicine and AI
AI's ability to analyze complex datasets allows for a more personalized approach to cancer treatment. By considering individual patient factors, AI algorithms can identify the most suitable therapies, minimizing adverse effects and maximizing efficacy. This targeted approach is a significant advancement in the field of oncology. This personalized medicine approach is crucial in enhancing treatment effectiveness and minimizing unnecessary treatments.
The Future of AI in Oncology
The future of AI in oncology is promising, with ongoing research focused on enhancing its capabilities. As AI systems become more sophisticated, they will likely play an even greater role in drug discovery, cancer prevention, and improving patient outcomes. Integrating AI into existing healthcare systems will be crucial for its widespread adoption and impact. The potential for AI to revolutionize cancer care is undeniable, and ongoing developments suggest a brighter future for patients facing this challenge.
Leveraging AI for Biomarker Identification and Analysis
AI-Powered Biomarker Discovery
Artificial intelligence (AI) is rapidly transforming the field of biomarker identification, offering unprecedented potential for accelerating the discovery process. AI algorithms can analyze vast datasets of genomic, proteomic, and clinical information to identify patterns and correlations that might be missed by traditional methods. This ability to sift through complex data allows researchers to pinpoint potential biomarkers with greater accuracy and speed, leading to a more efficient pipeline for preclinical and clinical trials.
By leveraging machine learning techniques, AI can identify novel biomarkers associated with specific cancers, treatment responses, or disease progression. This includes analyzing intricate relationships between genetic mutations, protein expression levels, and patient outcomes, ultimately enabling more precise and effective cancer therapies.
Advanced Data Analysis Techniques
AI algorithms excel at handling the complexities of modern biomedical datasets. These algorithms can incorporate diverse data types, including genomic sequences, imaging data, and clinical records. This integrated approach allows for a holistic view of the patient, enabling the identification of subtle patterns and relationships that might not be apparent with traditional methods. Advanced analysis techniques, such as deep learning, can further enhance the accuracy of biomarker identification.
Furthermore, AI can be used to identify and validate biomarkers across different patient populations and disease subtypes. This ability to analyze data from diverse sources allows for more generalizable and reliable biomarker identification, leading to potentially more effective treatments for a wider range of patients.
Clinical Implementation and Validation
The successful translation of AI-identified biomarkers into clinical practice requires rigorous validation and implementation strategies. This involves conducting carefully designed clinical trials to assess the performance of the identified biomarkers in predicting treatment outcomes and disease progression. Robust validation steps are crucial to ensure the reliability and clinical utility of these biomarkers in real-world settings.
Personalized Treatment Strategies
Once validated, AI-derived biomarkers can be incorporated into personalized treatment strategies. By analyzing individual patient data, AI can help clinicians determine the most effective treatment approach for each patient. This personalized approach to cancer treatment, based on specific biomarker profiles, holds significant promise for improving patient outcomes and reducing adverse effects. Such strategies can potentially lead to more targeted therapies, maximizing efficacy and minimizing unnecessary side effects.
Improving Diagnostic Accuracy and Efficiency
AI's ability to analyze complex data sets can significantly improve the accuracy and efficiency of cancer diagnostics. By identifying subtle patterns in medical images, genetic profiles, or clinical data, AI can assist clinicians in making more accurate diagnoses, leading to earlier interventions and potentially improved patient outcomes. This enhanced diagnostic accuracy and efficiency can be particularly valuable in resource-constrained settings, where access to specialized expertise is limited.
Predictive Modeling for Treatment Response and Outcomes
Understanding the Fundamentals of Predictive Modeling
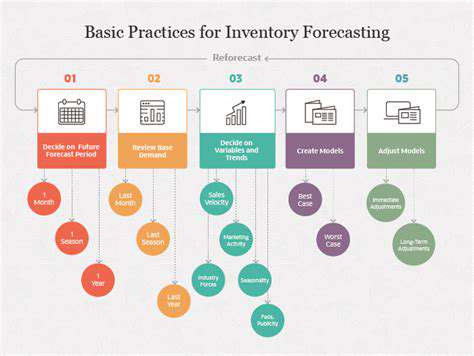
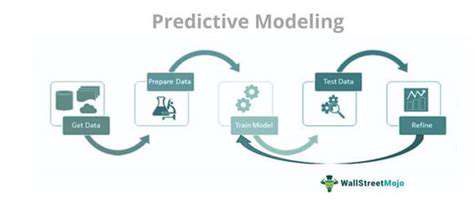
Predictive modeling, a powerful tool in healthcare, leverages historical data to anticipate future outcomes. By identifying patterns and relationships within this data, healthcare professionals can make more informed decisions regarding treatment strategies and patient care. This process involves the development of algorithms and statistical models that analyze various factors, such as patient demographics, medical history, and lifestyle choices, to predict the likelihood of specific health conditions or treatment responses. This approach ultimately aims to optimize treatment plans and improve patient outcomes.
The core principle behind predictive modeling is the identification of key indicators that correlate with specific health outcomes. This process requires careful consideration of data quality and the potential for bias. A thorough understanding of the variables influencing the outcome is crucial for developing accurate and reliable models. Robust statistical methods are employed to ensure that the models are not overfitting to the training data, which would lead to poor generalizability and inaccurate predictions.
Applying Predictive Modeling in Treatment Planning
Predictive models can significantly impact treatment planning by assisting in the selection of optimal therapies. For instance, a model trained on patient data might predict a patient's response to a specific medication, allowing clinicians to tailor treatments to individual needs and potentially improve treatment efficacy. By anticipating potential complications or adverse events, predictive models can help healthcare providers develop proactive strategies to mitigate risk.
Implementing these models can lead to more personalized and effective treatment strategies. This personalization can include selecting the most suitable treatment option, predicting the likelihood of success, and identifying patients who may require additional monitoring or support. Furthermore, predictive modeling can help in resource allocation by identifying patients who are most likely to benefit from specific interventions, leading to a more efficient use of healthcare resources.
The Role of Data in Predictive Modeling
The quality and quantity of data are paramount to the success of predictive modeling. Data should be comprehensive, encompassing relevant patient information, medical history, lifestyle factors, and treatment outcomes. Accurate and reliable data is essential for building accurate predictive models. Data collection procedures should be standardized and rigorous, minimizing bias and ensuring the validity and reliability of the findings. This ensures that the model's predictions are based on sound evidence and not on flawed or incomplete data.
Data preprocessing is a crucial step in preparing data for predictive modeling. This involves cleaning, transforming, and preparing data for analysis. This step includes handling missing values, converting categorical variables into numerical representations, and scaling numerical variables to a similar range. Thorough data preprocessing is essential for building reliable and accurate models.
Challenges and Considerations in Predictive Modeling
Despite the significant potential of predictive modeling, several challenges must be addressed. One key consideration is the potential for bias in the data, which could lead to inaccurate or unfair predictions. Careful attention must be paid to ensuring that the models are not perpetuating existing biases within the dataset. Another challenge lies in the complexity of the underlying biological systems, which can make it difficult to identify all the relevant factors influencing treatment outcomes.
Ethical considerations are paramount in the development and application of predictive models. The use of sensitive patient data necessitates strict adherence to privacy regulations and ethical guidelines. Transparency and explainability of the models are also critical to building trust and ensuring responsible use. Furthermore, ensuring model accuracy and avoiding overfitting to specific datasets are crucial aspects to consider.
Future Directions and Applications
The field of predictive modeling in healthcare is constantly evolving, with ongoing research exploring new methodologies and applications. Integration with emerging technologies, such as artificial intelligence and machine learning, holds significant potential for improving predictive accuracy and expanding the scope of applications. Further research is needed to explore the use of predictive models in various healthcare settings, from primary care to specialized treatments.
The future of predictive modeling lies in its ability to enhance patient care and improve healthcare outcomes. By providing clinicians with valuable insights, predictive models can contribute to a more proactive and personalized approach to healthcare, ultimately leading to better health for individuals and communities.