Introduction to AI in Clinical Trial Analysis
Understanding the Role of AI in Clinical Trials
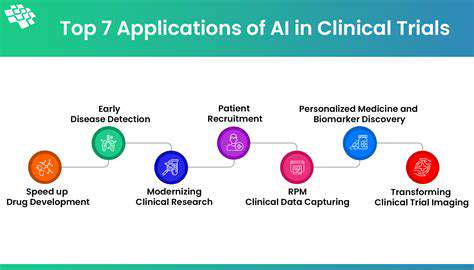
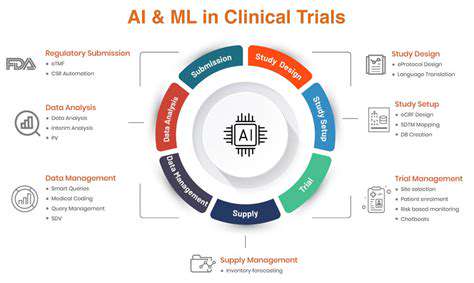
Artificial intelligence (AI) is rapidly transforming various sectors, and clinical trials are no exception. AI's ability to analyze vast datasets, identify patterns, and automate tasks is revolutionizing the way clinical trials are conducted, from study design and patient recruitment to data analysis and interpretation. This enhanced efficiency and accuracy promise to accelerate the development of new treatments and therapies, ultimately benefiting patients worldwide. AI-powered tools can significantly reduce the time and cost associated with clinical trials.
By automating tasks like data entry and analysis, AI can help researchers focus on more critical aspects of the trial process. This leads to a more streamlined workflow, minimizing errors and accelerating the overall timeline. Moreover, AI algorithms can identify potential biases in data, ensuring that trials are conducted with greater objectivity and fairness.
The implementation of AI in clinical trials also presents opportunities for personalized medicine. AI can analyze patient data to identify individuals who are most likely to benefit from a particular treatment, allowing for more targeted therapies. This personalized approach can lead to better treatment outcomes and a reduction in adverse events.
Challenges and Ethical Considerations
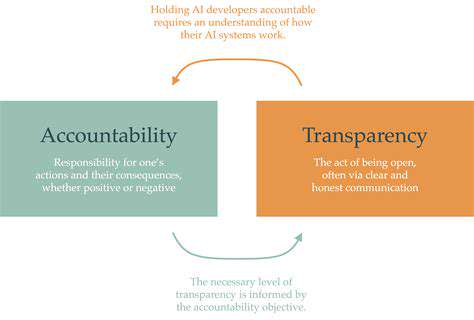
While the potential benefits of AI in clinical trials are substantial, several challenges and ethical considerations need careful consideration. One key concern is ensuring data security and privacy. Clinical trial data often contains sensitive patient information, and robust security measures must be in place to protect this data from unauthorized access. The need for transparency in AI algorithms is also crucial. Researchers need to understand how these algorithms arrive at their conclusions to ensure the validity and reliability of the results.
Another challenge involves the potential for bias in AI algorithms. If the training data used to develop these algorithms reflects existing societal biases, the AI tools may perpetuate and even amplify these biases in the clinical trial process. Carefully curated and diverse datasets are vital to mitigate this risk. The need for rigorous validation and testing of AI tools is paramount to prevent inaccurate predictions and potential harm to patients.
The ethical implications of using AI to make critical decisions in clinical trials need careful consideration. The potential for algorithmic bias and the need for human oversight in the decision-making process are crucial areas that need to be addressed. Questions around accountability and responsibility in case of errors or adverse outcomes must be carefully considered and addressed.
Ultimately, responsible and ethical implementation of AI in clinical trials will be essential to ensure that these powerful tools are used for the benefit of patients and contribute to the advancement of healthcare.
Advanced Statistical Modeling and Predictive Analytics
Statistical Modeling Techniques
Advanced statistical modeling plays a crucial role in analyzing clinical trial data and extracting meaningful insights. Various techniques are employed, ranging from linear regression for simple relationships to more complex models like logistic regression for binary outcomes. These models help us understand the relationships between treatment, patient characteristics, and clinical outcomes, such as disease progression or remission rates. Furthermore, generalized linear models (GLMs) provide flexibility for different types of outcome variables, while survival analysis models are essential for assessing time-to-event outcomes like disease-free survival.
Beyond these foundational techniques, more sophisticated methods like mixed-effects models are employed when dealing with hierarchical data structures, such as data from multiple centers or nested patient groups. These models account for the correlation between observations within the same group, leading to more accurate and reliable results.
Predictive Analytics for Trial Design
Predictive analytics is essential for optimizing clinical trial design and resource allocation. By analyzing historical data and patient characteristics, we can identify potential predictors of treatment response or adverse events. This allows researchers to stratify patients based on predicted risk factors, potentially leading to more efficient and effective trials with higher statistical power.
Predictive models can also help identify optimal sample sizes for different treatment groups, minimizing unnecessary participant exposure while maximizing the chance of detecting a meaningful treatment effect. This ultimately contributes to faster and more cost-effective clinical trials.
Machine Learning Algorithms in Clinical Trials
Machine learning algorithms, including support vector machines (SVMs), decision trees, and random forests, offer powerful tools for predictive modeling in clinical trials. These algorithms can identify complex patterns and relationships within the data that traditional statistical methods may miss. They can be applied to various tasks, from predicting treatment response to identifying potential biomarkers of disease.
Ensemble methods, such as random forests, are particularly useful for handling high-dimensional data and mitigating overfitting. These techniques can improve the accuracy and robustness of predictive models while reducing the risk of false positives or negatives.
Data Preparation and Feature Engineering
Accurate and reliable results from statistical modeling and predictive analytics heavily rely on the quality and preparation of the data. This includes cleaning the data, handling missing values, and transforming variables to improve model performance. Feature engineering is a crucial step where new variables are created from existing ones to capture more complex relationships and potentially enhance the predictive power of the models.
Careful consideration of data quality and appropriate feature engineering are essential steps in ensuring the validity and reliability of the results obtained from the advanced statistical modeling techniques.
Evaluating Model Performance and Validation
Rigorous evaluation of the performance of statistical models and predictive analytics is critical. Metrics such as accuracy, precision, recall, and F1-score are used to assess the model's ability to correctly classify or predict outcomes. Cross-validation techniques are employed to ensure that the model generalizes well to unseen data and avoids overfitting to the training dataset. This process helps researchers assess the model's robustness and reliability in real-world settings.
Handling Imbalanced Datasets
Clinical trials often involve imbalanced datasets, where the distribution of outcomes (e.g., success versus failure) is skewed. This can lead to biased models that perform poorly on the less frequent outcome. Special techniques, such as oversampling the minority class or using cost-sensitive learning, are used to address this challenge. These methods aim to improve the model's ability to accurately predict less frequent events, which are often of particular clinical importance.
Ethical Considerations in Predictive Modeling
The use of predictive modeling in clinical trials raises ethical considerations regarding patient privacy, data security, and potential biases in the models. Transparency and explainability of the models are essential to ensure that the results are understood and trusted by healthcare professionals and patients. Furthermore, the potential for discrimination based on patient characteristics needs careful consideration and mitigation strategies to ensure fairness and equitable access to treatment.
Improving Efficiency and Reducing Bias in Clinical Trial Design
Streamlining Processes
Improving efficiency often hinges on streamlining processes. This involves analyzing current workflows, identifying bottlenecks, and implementing changes to optimize the flow of tasks. By simplifying steps and eliminating redundant actions, businesses can significantly reduce wasted time and resources. This ultimately leads to a more productive and responsive operation.
A key aspect of streamlining is understanding the current process from start to finish. This includes identifying all the steps, the people involved, and the resources used. Once this is understood, areas where improvements can be made become apparent. A well-defined and streamlined process reduces errors and increases overall efficiency.
Optimizing Resource Allocation
Efficient resource allocation is crucial for maximizing productivity. It involves strategically assigning personnel, equipment, and materials to tasks in a way that aligns with business objectives. This careful allocation ensures that resources are utilized effectively, minimizing idle time and maximizing output. Poor resource allocation, on the other hand, can lead to bottlenecks and decreased productivity.
Effective resource allocation requires a clear understanding of the workload, skills required, and available resources. It's about matching the right resources to the right task at the right time. This requires ongoing monitoring and adjustments to ensure optimal performance.
Leveraging Technology
The integration of technology plays a vital role in enhancing efficiency. From automation tools to project management software, technology can streamline tasks, track progress, and improve communication. Embracing technology can significantly reduce manual effort and human error. This leads to quicker turnaround times and reduced costs in the long run.
Choosing the right technology is crucial. A carefully considered selection process ensures that the chosen tools are compatible with existing systems and workflows. Furthermore, training employees on new technologies is vital to ensure their effective use and integration.
Enhancing Communication
Effective communication is the cornerstone of any successful organization. Clear and concise communication ensures that everyone is on the same page, reduces misunderstandings, and fosters collaboration. Open communication channels facilitate the flow of information and ideas, leading to more informed decision-making. Poor communication can lead to confusion, delays, and ultimately, decreased productivity.
Establishing clear communication protocols and channels is essential for ensuring that information is disseminated effectively and efficiently. This includes regular meetings, clear documentation, and readily available resources for employees to access information.
Improving Training and Development
Investing in employee training and development is a critical aspect of improving efficiency. Training programs equip employees with the necessary skills and knowledge to perform their tasks effectively and efficiently. This leads to improved job performance and increased productivity. Without proper training, employees may struggle with their work leading to errors and wasted time.
Implementing Performance Metrics
Implementing performance metrics is essential for tracking progress and identifying areas for improvement. By establishing key performance indicators (KPIs), businesses can monitor productivity levels, identify bottlenecks, and measure the effectiveness of implemented changes. This data-driven approach helps to identify trends and areas needing attention, allowing for proactive interventions and improvements.
Regularly reviewing and analyzing performance metrics provides valuable insights into the effectiveness of strategies and interventions. This allows for adjustments to be made in real time, ensuring that strategies remain aligned with objectives and that optimal performance is consistently achieved.
Promoting a Positive Work Environment
A positive and supportive work environment is essential for fostering productivity and efficiency. This includes promoting teamwork, encouraging collaboration, and recognizing and rewarding employees for their contributions. A positive atmosphere reduces stress and improves morale, resulting in a more engaged and productive workforce. A negative work environment, on the other hand, can lead to decreased motivation and decreased efficiency.
Investing in employee well-being, fostering a culture of recognition, and promoting a healthy work-life balance are all crucial components of creating a positive and productive work environment. This environment is conducive to innovation and high performance.
The Future of AI in Clinical Trial Outcome Analysis
Accelerated Drug Discovery and Development
Artificial intelligence (AI) is poised to revolutionize the clinical trial process, leading to faster and more efficient drug discovery and development. By analyzing vast datasets of biological and clinical information, AI algorithms can identify promising drug candidates at an unprecedented speed, drastically reducing the time and resources required for traditional methods. This accelerated pace is crucial for addressing pressing global health challenges. This includes identifying potential side effects and interactions at earlier stages, saving both time and money.
AI's ability to sift through mountains of data enables researchers to pinpoint patterns and correlations that might be missed by human observation. This data-driven approach promises to lead to more targeted therapies and personalized medicine, ultimately improving patient outcomes.
Personalized Treatment Strategies
AI can analyze individual patient data, including genetic information, medical history, and lifestyle factors, to tailor treatment plans. This personalized approach is critical for maximizing the effectiveness of therapies and minimizing adverse reactions. By understanding a patient's unique biological makeup, AI can suggest therapies that are most likely to succeed while mitigating the risk of harmful side effects.
This level of individualized care is particularly important in complex diseases where one-size-fits-all approaches often fail. AI can identify the specific genetic markers or biomarkers that predict a patient's response to a particular treatment, allowing clinicians to make informed decisions.
Improved Trial Design and Recruitment
AI can optimize clinical trial design by predicting patient enrollment rates and identifying potential biases in the selection process. This allows for more efficient allocation of resources and ensures that trials are representative of the broader patient population, leading to more reliable results. By streamlining the trial process, AI can significantly reduce the time and cost associated with these studies.
Enhanced Data Analysis and Interpretation
AI algorithms can analyze and interpret complex clinical trial data with exceptional speed and accuracy. This sophisticated analysis can uncover patterns and relationships that might be missed by conventional methods. The ability to extract meaningful insights from vast datasets is crucial for understanding treatment efficacy and safety.
Increased Efficiency in Data Management
AI can automate the tedious and time-consuming tasks involved in clinical trial data management, such as data entry, validation, and standardization. This automation frees up researchers to focus on more strategic aspects of the trial process, like analyzing data and designing new experiments.
Ethical Considerations and Challenges
The increasing use of AI in clinical trials raises important ethical considerations regarding data privacy, bias in algorithms, and the potential for misinterpretation of results. Careful attention must be paid to ensuring that AI systems are developed and deployed in a responsible and ethical manner. These crucial issues require careful consideration and thoughtful solutions.
Regulatory Landscape and Adoption
Establishing clear regulatory guidelines for the use of AI in clinical trials is essential to ensure the safety and efficacy of new treatments. The development of robust regulatory frameworks will foster trust and adoption within the medical community. This will ultimately enable the broader implementation of AI-powered solutions in the clinical trial process.