A Revolutionary Approach
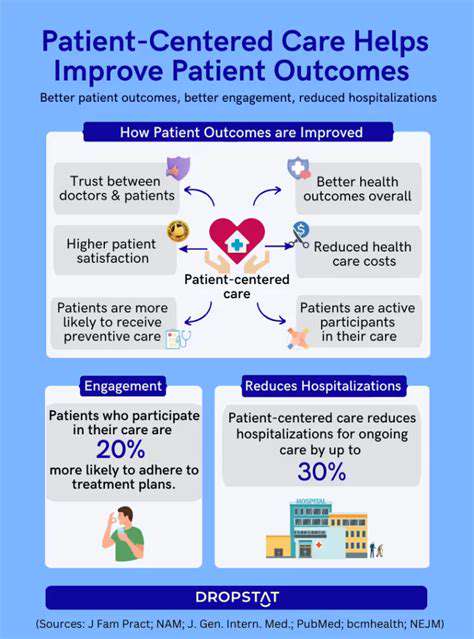
Automated disease detection is rapidly transforming healthcare, offering the potential to revolutionize diagnosis and treatment. This technology promises quicker and more accurate diagnoses, enabling early intervention and potentially saving lives. The ability to analyze vast datasets of medical images and patient data allows for the identification of patterns and anomalies that might be missed by human clinicians. Early detection is crucial in many diseases, significantly improving patient outcomes.
By automating the process, healthcare systems can potentially reduce diagnostic delays, and streamline the workflow. This efficiency can lead to lower costs and increased accessibility to critical medical services for a wider population.
Machine Learning Algorithms: The Engine of Automation
The core of automated disease detection lies in machine learning algorithms, which are trained on large datasets of medical images, patient records, and other relevant data. These algorithms learn to identify patterns and anomalies associated with different diseases, allowing for accurate and efficient diagnosis.
Sophisticated algorithms like deep learning models excel at analyzing complex medical images, such as X-rays, CT scans, and MRIs, to detect subtle indicators of diseases like cancer, cardiovascular issues, and neurological disorders. These algorithms are continuously evolving, becoming more accurate and efficient with each iteration.
Image Analysis for Precision Diagnosis
Medical imaging plays a crucial role in automated disease detection. Techniques like computer vision and image processing are used to analyze images, extracting valuable information about the structure and function of organs and tissues. This analysis helps to identify potential abnormalities and indicators of disease.
The ability to analyze images at a pixel level allows for greater precision in diagnosis, leading to earlier and more accurate detection of diseases. This is particularly important for conditions that may have subtle or non-obvious symptoms in their early stages.
Data Security and Privacy Considerations
As automated disease detection systems rely heavily on patient data, robust security measures are essential to protect sensitive information. Data encryption, access controls, and compliance with privacy regulations like HIPAA are critical to ensure the confidentiality and integrity of patient records.
Protecting patient data is paramount, and strict adherence to ethical guidelines and regulations is vital for the responsible development and deployment of these technologies. This ensures public trust and confidence in the use of automated systems in healthcare.
Clinical Validation and Integration
The accuracy and reliability of automated disease detection systems must be rigorously validated through clinical trials and real-world testing. This involves comparing the system's diagnoses to those of experienced clinicians, ensuring the system's performance meets high standards of accuracy and precision.
Successful integration into existing healthcare workflows is crucial for effective implementation. This includes addressing practical concerns like compatibility with existing imaging equipment and electronic health record systems, ensuring seamless data flow and efficient utilization of the system.
Cost-Effectiveness and Accessibility
Automated disease detection systems, while initially requiring significant investment, can ultimately prove cost-effective over time by reducing diagnostic errors, accelerating treatment, and potentially lowering healthcare costs. The potential for increased accessibility to specialized diagnostic services is another key benefit.
Improved access to early diagnosis and treatment, especially in underserved communities, is a significant positive outcome of these technologies. Lower costs and faster diagnoses can lead to better health outcomes and reduce the burden on healthcare systems.
Future Directions and Research
Future research in automated disease detection is focused on developing more sophisticated algorithms, expanding the types of diseases that can be detected, and improving the integration of these systems into clinical practice. The goal is to enhance diagnostic accuracy, speed, and accessibility for a wide range of medical conditions.
Ongoing research will further refine these technologies and expand their capabilities, leading to even more precise and efficient disease detection in the future. This includes exploring the use of artificial intelligence to predict disease risk and personalize treatment strategies.
AI's Role in Forecasting Patient Outcomes
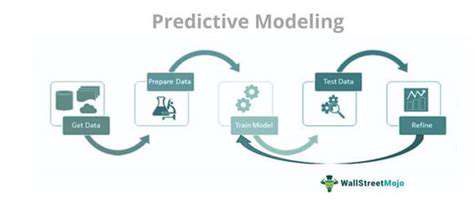
AI-powered predictive modeling is revolutionizing healthcare by enabling the forecasting of patient outcomes. By analyzing vast datasets encompassing patient history, medical imaging, lifestyle factors, and genetic information, AI algorithms can identify patterns and predict the likelihood of specific health conditions developing or worsening. This capability is invaluable for proactive interventions, enabling healthcare providers to tailor treatment plans and preventative measures to individual patient needs, ultimately enhancing patient care and potentially improving overall public health outcomes. The potential for early disease detection and personalized treatment pathways is immense.
Improving Diagnostic Accuracy through Predictive Models
Predictive models can significantly augment diagnostic accuracy in healthcare. By leveraging historical data and integrating various factors, these models can identify subtle patterns and anomalies that might be missed by human clinicians. This increased accuracy translates to earlier diagnoses, enabling timely interventions and potentially improving treatment efficacy. Imagine a system that can analyze a patient's MRI scan and predict the likelihood of a specific pathology, alerting the physician to potential issues well before they manifest clinically. This early warning system is a game-changer for the future of patient care.
Personalized Treatment Strategies Based on Predictions
AI-driven predictive modeling has the potential to personalize treatment strategies for individual patients. By considering a patient's unique characteristics and predicted response to different therapies, AI can recommend optimal treatment plans. This level of personalization is crucial for improving treatment outcomes and reducing adverse effects, as it ensures that the most effective and safest interventions are tailored to the specific needs of each patient. The potential to optimize treatment decisions and minimize the risk of adverse events is a major benefit of this approach.
Enhancing Resource Allocation and Efficiency
Predictive models can optimize resource allocation and streamline healthcare operations. By anticipating patient needs, hospitals and clinics can better manage staffing levels, allocate resources more effectively, and reduce wait times. For example, anticipating the need for intensive care beds based on predicted patient acuity levels allows for proactive resource allocation, minimizing potential bottlenecks and improving the overall efficiency of the healthcare system. This is crucial for managing costs and ensuring equitable access to care for all.
Ethical Considerations and Future Directions
While AI-driven predictive modeling holds immense promise for healthcare, it's essential to address the ethical implications associated with its use. Issues such as data privacy, bias in algorithms, and the potential for misinterpretation of predictions need careful consideration. Future research should focus on developing robust methods for mitigating bias, ensuring data security, and establishing clear guidelines for the responsible application of these technologies. The integration of human oversight and ethical frameworks is critical for responsible AI implementation in healthcare, ensuring that these powerful tools are used to benefit patients and society as a whole.